| Name | Clomipramine Hydrocloride |
| Classes |
Central Nervous System Agent Psychotherapeutic Agent Tricyclic Antidepressant |
| Diseases |
Depression Fear Mental Disorder Repetative Behavior |
Clomipramine Hydrocloride
Clomipramine Hydrochloride belongs to a class of drugs called the tricyclic antidepressants. Its main mode of action is to prevent serotonin and norepinephrine from being reabsorbed, so increasing their levels in the brain.
Clomipramine Hydrochloride is indicated for Obsessive compulsive disorder & depression.
- Starting dose: Starting at 25 mg daily, as with adults, the dose should be gradually raised (also in divided doses with meals to decrease gastrointestinal side effects) over the first two weeks, as tolerated, up to a daily maximum of 3 mg/kg or 100 mg, whichever is lower. Following that, the dosage may be gradually raised over the next few weeks, up to a daily maximum of 3 mg/kg or 200 mg, whichever is less. After titration, the complete daily dose may be given once daily at bedtime to minimize daytime sedation, much as it is for adults.
- Maintenance dose: While there are no systematic studies that answer the question of how long to take Clomipramine, OCD is a chronic disorder, and it is fair to maintain treatment if the patient is responding. Despite the lack of evidence of Clomipramine's efficacy after 10 weeks in controlled trials, patients have been kept on the drug for up to a year under double-blind settings with no loss of benefit. However, dosage modifications should be made to keep the patient on the lowest effective dose, and patients should be reviewed on a regular basis to see whether treatment is still necessary. The complete daily dose can be administered once a day at bedtime during maintenance.
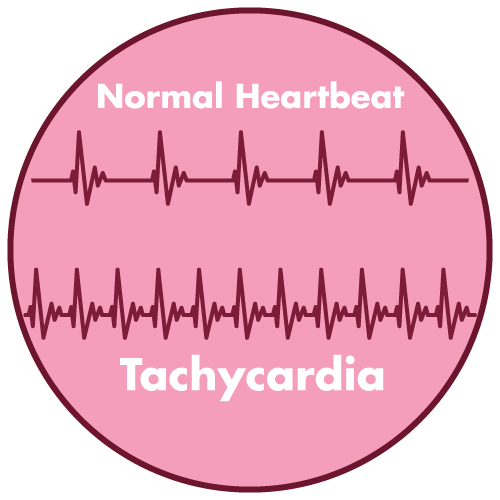
- Cardiovascular: Orthostatic hypotension, hypertension, tachycardia, palpitation, myocardial infarction, arrhythmias, heart block, ECG changes, precipitation of congestive heart failure, stroke.
- Psychiatric: Confusional states (especially in the elderly) with hallucinations, disorientation, delusions; anxiety, restlessness, agitation; insomnia and nightmares; hypomania; exacerbation of psychosis.
- Neurological: Numbness, tingling, paresthesias of extremities; incoordination, ataxia, tremors; peripheral neuropathy; extrapyramidal symptoms; seizures, alterations in EEG patterns; tinnitus.
- Anticholinergic: Dry mouth, and, rarely, associated sublingual adenitis; blurred vision, disturbances of accommodation, mydriasis; constipation, paralytic ileus; urinary retention, delayed micturition, dilation of the urinary tract.
- Allergic: Skin rash, petechiae, urticaria, itching, photosensitization; edema (general or of face and tongue); drug fever; crosssensitivity with desipramine.
- Hematologic: Bone marrow depression including agranulocytosis; eosinophilia; purpura; thrombocytopenia.
- Gastrointestinal: Nausea and vomiting, anorexia, epigastric distress, diarrhea; peculiar taste, stomatitis, abdominal cramps, black tongue.
- Endocrine: Gynecomastia in the male; breast enlargement and galactorrhea in the female; increased or decreased libido, impotence; testicular swelling; elevation or depression of blood sugar levels; inappropriate antidiuretic hormone (ADH) secretion syndrome.
- Other: Jaundice (simulating obstructive); altered liver function; weight gain or loss; perspiration; flushing; urinary frequency; drowsiness, dizziness, weakness and fatigue; headache; parotid swelling; alopecia; proneness to falling.
- Withdrawal Symptoms: Though not indicative of addiction, abrupt cessation of treatment after prolonged therapy may produce nausea, headache, and malaise.
- Depression is linked to a higher risk of suicidal ideation, self-harm, and suicide (suicide-related events). This danger exists until there is a major remission. Because improvement may not emerge for several weeks or longer after starting treatment, patients should be constantly followed until they do. Suicide risk may increase in the early stages of recovery, according to clinical experience.
- Other psychiatric illnesses for which clomipramine is treated have also been linked to an increased risk of suicide. Furthermore, these issues could be co-morbid with major depressive disorder. When treating individuals with different mental diseases, the same care should be used as when treating patients with major depressive disorder.
- Patients with a history of suicidal ideation or a significant degree of suicidal ideation prior to treatment are known to be at a higher risk of suicidal thoughts or suicide attempts and should be closely monitored during treatment. A meta-analysis of placebo-controlled clinical trials of antidepressant drugs in adult patients with psychiatric disorders found that antidepressants were associated with an increased risk of suicidal behavior in patients younger than 25 years old when compared to placebo.
- Close monitoring of patients, particularly those at high risk, should accompany drug therapy, particularly during the early stages of treatment and after dose changes.
- Patients (and caregivers of patients) should be alerted about the need to monitor for any clinical worsening, suicidal behaviour or thoughts and unusual changes in behaviour and to seek medical advice immediately if these symptoms present. Patients with depressive disorders, both adult and paediatric, may experience worsening of depression and/or suicidality or other psychiatric symptoms, whether or not they are taking antidepressant medication.
Contraindication
- Contraindicated in patients hypersensitive to any component of the medication.
- Concomitant administration with Monoamine oxidase inhibitors is contraindicated; such as-
None known.
The drug is contraindicated during the acute recovery period after a myocardial infarction.
 Bangla
Bangla English
English