| Name | Heparin Sodium |
| Classes |
Anticoagulant Coagulation Modifier Haematological Agent |
| Diseases |
Cardiovascular Disease Pulmonary Embolism |
Heparin Sodium
Heparin Sodium is an anticoagulant. Heparin interacts with the naturally occurring plasma protein Antithrombin III to induce a conformational change that significantly increases Antithrombin III's serine protease activity, inhibiting the activated coagulation factors involved in the clotting cascade, particularly Xa and IIa. Heparin inhibits Factor Xa in small doses and thrombin in larger doses (Factor IIa). Heparin also inhibits the activation of the fibrin stabilizing factor, which prevents the formation of a stable fibrin clot. Heparin lacks fibrinolytic activity and thus will not lyse existing clots.
Heparin sodium is indicated for:
- Prophylaxis and treatment of venous thromboembolism and pulmonary embolism
- Atrial fibrillation with embolization
- Treatment of acute and chronic consumptive coagulopathies (disseminated intravascular coagulation)
- Prevention of clotting in arterial and cardiac surgery
- Prophylaxis and treatment of peripheral arterial embolism
- Anticoagulant use in blood transfusions, extracorporeal circulation, and dialysis procedures.
Recommended Adult Dosages:
| Intermittent Intravenous Injection | Initial Dose | 10,000 units |
| Every 4 to 6 hours | 5,000 to 10,000 units | |
| Continuous Intravenous Infusion | Initial Dose | 5,000 units by intravenous injection |
| Continuous | 20,000 to 40,000 units/24 hours |
Surgery of the Heart and Blood Vessels: Intravascular via Total Body Perfusion
- Initial Dose: ≥ 150 units/kg; adjust for longer procedures
Extracorporeal Dialysis : Intravascular via Extracorporeal Dialysis
- Follow equipment manufacturer’s operating directions carefully.
Pediatric Use :
- Initial Dose: 75 to 100 units/kg (intravenous bolus over 10 minutes)
- Maintenance Dose
- Infants: 25 to 30 units/kg/hour;
- Infants < 2 months have the highest requirements (average 28 units/kg/hour)
- Children > 1 year of age: 18 to 20 units/kg/hour; Older children may require less heparin, similar to weight-adjusted adult dosage
- Monitoring: Adjust heparin to maintain aPTT of 60 to 85 seconds, assuming this reflects an anti-Factor Xa level of 0.35 to 0.70.
Most common adverse reactions are-
- hemorrhage
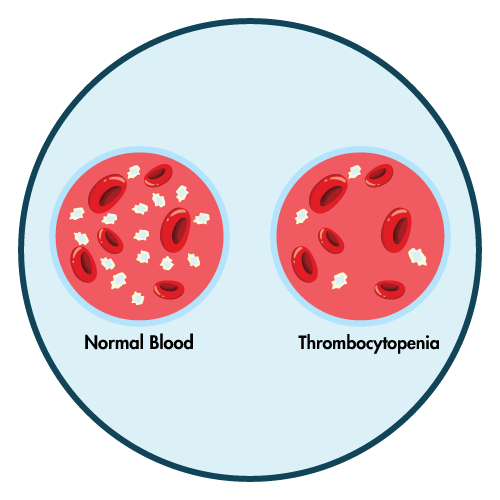
- thrombocytopenia
- HIT and HITT
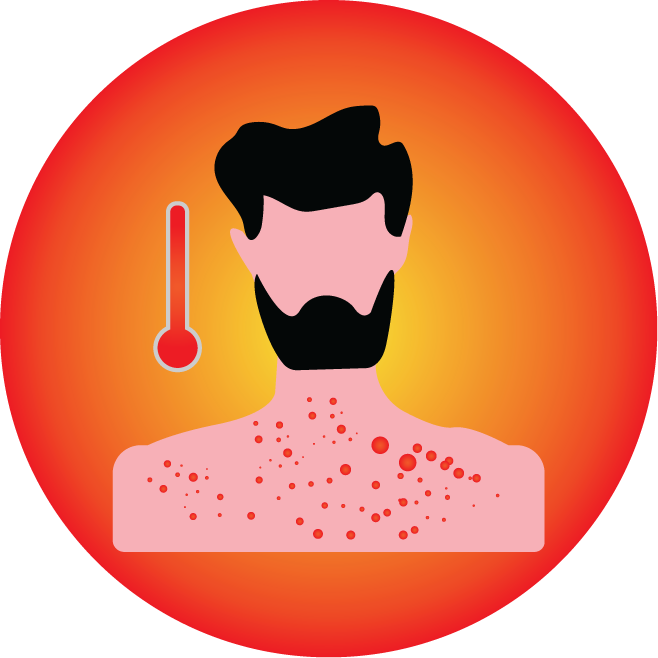
- hypersensitivity reactions
- elevations of aminotransferase levels
- heparin resistance
- Fatal Medication Errors: Confirm choice of correct strength prior to administration.
- Hemorrhage: Fatal cases have occurred. Use caution in conditions with increased risk of hemorrhage.
- Heparin-Induced Thrombocytopenia (HIT) and Heparin-Induced Thrombocytopenia and Thrombosis (HITT): Monitor for signs and symptoms and discontinue if indicative of HIT and HITT.
- Monitoring: Blood coagulation tests guide therapy for full-dose heparin. Monitor platelet count and hematocrit in all patients receiving heparin.
- Heparin Resistance: Increased resistance to heparin is frequently encountered in fever, thrombosis, thrombophlebitis, infections with thrombosing tendencies, myocardial infarction, cancer, in postsurgical patients, and patients with antithrombin III deficiency.
- Hypersensitivity: Because heparin sodium is derived from animal tissue, monitor for signs and symptoms of hypersensitivity when it is used in patients with a history of allergy.
Contraindication
Contraindicated in patients with known hypersensitivity to heparin or pork products.
None known.
Heparin is contraindicated in the following groups of patients-
- History of Heparin-Induced Thrombocytopenia (HIT) and Heparin-Induced Thrombocytopenia and Thrombosis (HITT)
- An uncontrolled bleeding state except when this is due to disseminated intravascular coagulation.
- In whom suitable blood coagulation tests- e.g., the whole blood clotting time, partial thromboplastin time, etc., cannot be performed at appropriate intervals (this contraindication refers to full-dose heparin; there is usually no need to monitor coagulation parameters in patients receiving low-dose heparin)
 Bangla
Bangla English
English